ICD codes are used primarily for diagnosing a patient, whereas CPT codes are used to support the diagnosis with the necessary medical treatment. Another tip for submitting claims properly is to familiarize yourself with common claims forms that many insurance companies use, such as the UB-04 form. This form is usually reserved for mental health clinics and specialized health centers for medical billing. The UB-04 and other mental health forms are uploaded on some compliant software programs, making it easier for you to electronically fill out and file the form. Our mental health insurance billing staff is on call Monday – Friday, 8am-6pm to ensure your claims are submitted and checked up on with immediacy. Following that, mental health providers must meticulously document the services rendered during each treatment session or psychiatric examination.
Ensure that the patient information is true. Double check!
After this process, you have all of the information required to file claims, what to charge your client when they come in for a visit and how to file their claim via online or otherwise. You’ll receive this data whether or not the claims you submitted went through or came back as a denial. If you’re enrolled with your payer to receive the status of the claims you submit through your clearinghouse or by other computerized means, you’re receiving electronic admittance advice (ERA). Essentially, you submit your claims to a clearinghouse, it runs your submission through a series of automated tests and alerts you to any errors.

Ask How to Bill Claims Online

If you don’t do it, you could surprise your patient later with an unexpected bill. Payers and clearinghouses will allow you to track electronically-submitted claims on a user dashboard. Third-party billing services should provide https://www.bookstime.com/blog/airbnb-accounting-and-bookkeeping you with regular status reports. If you’re new to mental health billing, you may feel overwhelmed, uncertain, or anxious about the process. Most mental health experts aren’t trained to navigate the medical billing landscape.
Account for Paid EOBs and Refile Denied Claims
This mental health insurance billing for dummies guide is just simply not the place to explain the vast number of ways that billing plays out. We recommend seeking professional help online research, a colleague, course, or through delegation. Once the services have been properly documented, ASP RCM Coders will issue CPT (Current Procedural Terminology) codes to each.
- We recommend reading and using Barbara Griswald’s book Navigating the Insurance Maze as a primer on how to submit paper claims correctly.
- Each modifier applies to certain CPT codes (shown on the far right column).
- This is yet one more reason why mental health providers choose billing services like TheraThink to help.
- Larger practices will need to carefully consider their budget and the number of full and part-time staff they can afford to hire based on their provider numbers.
- This step happens simultaneously with step 4, but it needs mentioning because it’s another added benefit of choosing the “most ideal” alternative.
Depending on that, the insurance covers a part or in some cases the whole of the coverage. Once the client’s eligibility and benefits are confirmed, proceed with the scheduled mental health session. During the session, ensure accurate documentation of the services provided, including the date, duration, and nature of the session.
Create and Submit Your Claim

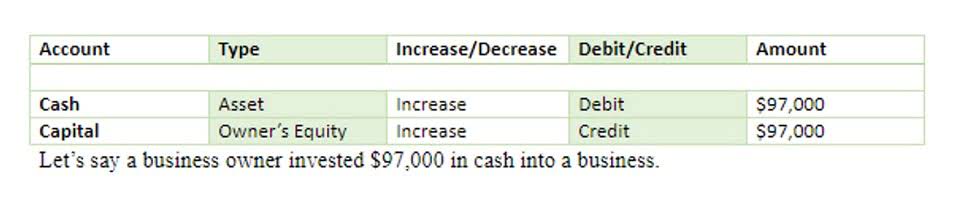
This should be applied effectively to lower the likelihood of claim rejections. And understanding these codes is critical for accurate invoicing and reimbursement. As already mentioned in this article, Verification of Benefits is a crucial aspect to ensure the patient’s insurance coverage details and the kind of services that they have intended to encounter. Refer to the table below to find the correct license level modifier to use when coding modifiers for your behavioral health insurance claims. When you send claims to payers, you need to properly monitor patient information, codes, regulations, and other critical details.
International Medical Graduate experience in medicine
The EHR you’re using probably isn’t the same one that a pediatrician’s private practice utilizes. Both EHRs serve different niche’s within the healthcare industry so they probably also have different features. That shouldn’t be a roadblock to integrating with a clearinghouse provider. It’s likely that the bulk of the solution provider’s clients are doctor’s offices.
Lighten your load with a solid EHR

When incorrect information or typos sneak into the initial patient records, those mistakes will appear on every bill until you realize there’s a problem. Since behavioral health providers see patients repeatedly, you may have multiple bills to correct and re-file thanks to one careless moment at the beginning. CPT codes communicate services and tasks performed by mental health professionals during sessions.
Or hire a billing service, submit your weekly appointments in 10 minutes, and focus on your private practice. You are to charge them after the fact for their patient responsibility payment per session as listed mental health billing for dummies on the completed EOB your receive from filing your claims. Now it’s time to verify their insurance coverage and your network status in their plan, then their benefits based on all of that, via a phone call.
- The representative may be able to assist you with the solution that will result in a payment.
- It is very important to ensure that attention is paid to differentiation within the CPT codes and the apt usage of codes to avoid any repercussions.
- As already mentioned in this article, Verification of Benefits is a crucial aspect to ensure the patient’s insurance coverage details and the kind of services that they have intended to encounter.
- Gathering the information from your clients is only the first step, it’s also your responsibility to ensure that it’s accurate, up-to-date and eligible.
